Introduction: The Silent Crisis of Empirical Prescribing
For decades, the standard medical approach to common infections—Urinary Tract Infections (UTIs), wound infections, or persistent fevers—was “empirical prescribing.” A doctor would look at the symptoms, guess the likely bacteria, and prescribe a broad-spectrum antibiotic. This “fire-and-forget” method saved time, but it has contributed to one of the greatest biological threats of the 21st century: Antimicrobial Resistance (AMR).
Today, the era of guessing is ending. Advanced diagnostic microbiology, specifically the Culture and Sensitivity (C&S) test, has moved from being a “specialist” tool to a primary necessity. Whether it is a catheter-associated infection in a hospital or a recurring boil in an outpatient setting, the “Culture” test is the only way to distinguish between a treatable infection and a resistant “superbug.”
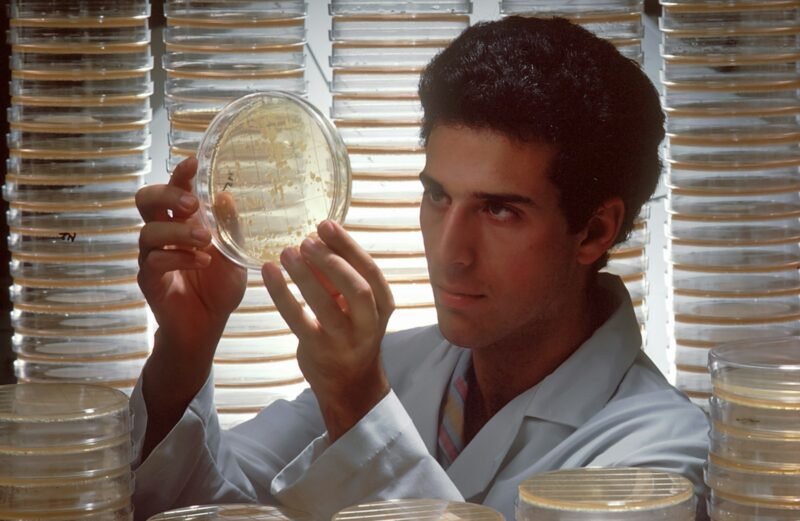
The Science of “The Culture”: Growing the Enemy A “Culture” is not simply looking at a sample under a microscope. It is a biological farming process. When a sample (urine, pus, sputum, or catheter tip) arrives at the lab, it is inoculated onto nutrient-rich agar plates (such as Blood Agar or MacConkey Agar).
-
Isolation: The goal is to grow “Colony Forming Units” (CFUs). By isolating a pure colony of the bacteria, the lab can identify the exact species.
-
Differentiation: Is it E. coli? Klebsiella? Pseudomonas? Knowing the name of the enemy is half the battle. For instance, Pseudomonas aeruginosa naturally repels many common antibiotics due to its unique cell wall structure, meaning standard drugs like Amoxicillin are useless against it before treatment even begins.
The “Sensitivity” Ring: How We Choose the Weapon Once the bacteria are grown, the “Sensitivity” (or Susceptibility) phase begins. This is often visualized using the Kirby-Bauer Disk Diffusion method. Small paper disks impregnated with different antibiotics are placed on the bacterial lawn.
-
The Zone of Inhibition: If the antibiotic works, it kills the bacteria around the disk, creating a clear “halo” or zone of inhibition.
-
MIC (Minimum Inhibitory Concentration): Modern automated systems go further, calculating the MIC—the lowest concentration of a drug needed to stop bacterial growth. This allows doctors to prescribe the minimum effective dose, reducing side effects and toxicity.
The “Catheter” Conundrum: Infection vs. Colonization One of the most complex areas of modern medicine is managing patients with indwelling catheters (tubes used to drain urine). Catheters are prone to biofilm formation—a slimy protective layer that bacteria build to hide from the immune system.
The Critical Distinction: A positive culture from a catheter bag doesn’t always mean infection. It might be “colonization” (bacteria living there peacefully).
-
The “Sample Port” Rule: This is why our lab rejects urine taken from the drainage bag. We require samples from the sterile catheter port or the Catheter Tip itself.
-
Biofilm Resistance: Research shows that bacteria in biofilms (like Staphylococcus epidermidis) can be 1,000 times more resistant to antibiotics than free-floating bacteria. A Catheter Tip Culture helps distinguish whether the source of the fever is the tube itself (requiring removal) or the bladder (requiring drugs).
The Rise of ESBLs and CREs Why is this testing so urgent? We are seeing a massive rise in specific resistant enzymes:
-
ESBL (Extended-Spectrum Beta-Lactamases): Enzymes produced by common gut bacteria (like E. coli) that destroy penicillin and cephalosporins.
-
CRE (Carbapenem-Resistant Enterobacteriaceae): The “nightmare bacteria” that are resistant even to Carbapenems, the “last resort” antibiotics.
Without a culture report, a doctor might prescribe a standard antibiotic for an ESBL infection. The drug will fail, the bacteria will multiply, and the patient may progress to sepsis. The C&S report acts as a radar system, detecting these enzymes early so the doctor can switch to specialized alternatives (like Fosfomycin or Meropenem) immediately.
Conclusion The “Culture” test is often annoying to patients because it takes 48–72 hours. In an age of instant gratification, waiting three days for a drug seems archaic. However, that wait is the price of precision. Treating a resistant infection with the wrong drug is not just useless; it is actively harmful, wiping out the body’s “good” bacteria while leaving the superbug to thrive.