Introduction: The Rise of the Super-Bug
Tuberculosis (TB) is an ancient disease, but the pathogen we are fighting today, Mycobacterium tuberculosis, is evolutionarily distinct from the bacteria of the past. We are currently witnessing the proliferation of MDR-TB (Multi-Drug Resistant TB) and XDR-TB (Extensively Drug-Resistant TB)—strains that have mutated to evade the antibiotics that have served as the standard of care for half a century.
For patients with a persistent cough, the traditional approach of “diagnose and treat” is no longer sufficient or safe. The new standard of care is “diagnose, profile, and treat.” This shift emphasizes the critical role of advanced Susceptibility Testing (DST) in preventing treatment failure and stopping the spread of resistant strains.
The Biology of Resistance: How TB Hides
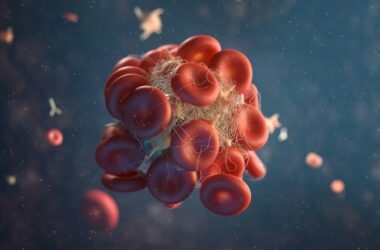
TB bacteria are notoriously difficult to kill. They are slow-growing and possess a thick, waxy cell wall rich in mycolic acid that repels many common antibiotics. Resistance occurs when a patient takes medication inconsistently or stops too early. The “weak” bacteria die off, but the sub-population of bacteria possessing random genetic mutations survives. These survivors multiply, creating a new colony that is immune to the drugs used.
The “Fallacy of Fitness” Historically, researchers believed that drug-resistant TB strains were “weaker” or less “fit” than normal TB, meaning they wouldn’t spread as easily. Findings from 2023 have shattered this myth. Modern MDR-TB strains have developed “compensatory mutations” that restore their biological fitness. This means a resistant strain can be just as infectious and aggressive as a standard strain. Consequently, a person can contract primary MDR-TB from a cough in a public space without ever having taken TB drugs themselves.
Why the “10-Drug Panel” is the New Gold Standard
Standard TB treatment involves a four-drug regimen: Isoniazid, Rifampicin, Ethambutol, and Pyrazinamide (HRZE). However, resistance to Isoniazid—the backbone of this regimen—is becoming increasingly common and often goes undetected. If a patient with hidden Isoniazid resistance is placed on the standard regimen, they are effectively receiving “monotherapy” (relying solely on the other drugs), which creates an environment that breeds further resistance, potentially leading to MDR-TB.
This is why the Acid Fast Susceptibility – 10 Drug Panel is essential. Using the WHO-endorsed BACTEC MGIT (Mycobacteria Growth Indicator Tube) system, laboratories can now test against a comprehensive profile.
The Technology: BACTEC MGIT Unlike old-fashioned solid media cultures that took 6 to 8 weeks to show results, the BACTEC MGIT system uses liquid culture media with a fluorescence indicator. As the bacteria grow and consume oxygen, the tube glows under UV light. This automated monitoring detects growth in days rather than months.
The 10-drug panel tests not only the first-line drugs but also the “second-line” defense, including fluoroquinolones (like Levofloxacin and Moxifloxacin) and injectable agents. This is vital because the latest WHO guidelines recommend new, shorter, all-oral regimens (such as BPaL: Bedaquiline, Pretomanid, Linezolid) for resistant TB. However, these potent drugs cannot be prescribed safely without confirming susceptibility first. Blind treatment with these agents can be disastrous.
The Phenomenon of “Heteroresistance”
Recent microbiology research has highlighted the danger of “heteroresistance.” This occurs when a patient hosts two distinct populations of TB bacteria in their lungs simultaneously: one sensitive to antibiotics and one resistant.
Standard smear microscopy (ZN Stain) cannot distinguish between these populations. It simply sees “bacteria.” Only a high-sensitivity Culture and Susceptibility test allows the laboratory to grow the bacterial population and expose it to drugs to see if a resistant sub-population exists. Identifying this “micro-resistance” early prevents months of ineffective treatment and lung damage.
Conclusion: Precision Medicine for TB
TB is no longer a simple infection; it is a complex genetic battle. The Susceptibility Test acts as a strategic war room, identifying exactly which weapons will eliminate the infection and which will be ineffective. For the patient, this means the difference between a 6-month cure and a 2-year struggle with resistant disease.
Tuberculosis Testing